Introduction: Allogeneic hematopoietic stem cell transplantation (allo-SCT) is a potentially curative treatment for many hematological malignancies and disorders. However, this potential is often impeded by several factors including relapse of the underlying disease, graft-vs-host disease (GVHD) and infectious complications. Specifically, acute GVHD continues to be a major factor in the morbidity and mortality of patients. Hence, the practice of allo-SCT is continuously evolving to mitigate these factors. In particular, advances in the conditioning regimens, GVHD prophylaxis, infectious disease monitoring and prophylaxis and supportive care not only have resulted in improved outcomes, but also have expanded potential indications for allo-HSCT. Therefore, we conducted a retrospective analysis on patients who underwent allo-SCT at The Ohio State University from 1986-2018 to better understand how survival has changed longitudinally in accordance with these therapeutic advancements.
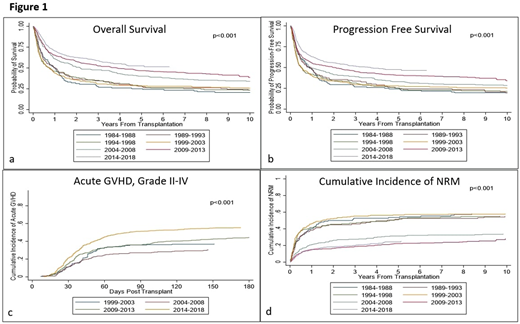
Method: We analyzed data from 1943 consecutive patients who received an allo-SCT. Patients were divided into seven groups based on the year of transplant: groups (gp) 1: 1984-1988, 2: 1989-1993, 3: 1994-1998, 4: 1999-2003, 5: 2004-2008, 6: 2009-2013, and 7: 2014-2018. The primary endpoints were overall survival (OS) and progression free survival (PFS), and log-rank test was used to compare across transplant years. The Kaplan-Meier method was used to estimate OS and PFS. The secondary endpoints were the cumulative incidences of grade II-IV and grade III-IV acute GVHD (aGVHD), chronic GVHD (cGVHD), and non-relapse mortality (NRM). Cumulative incidence rates were estimated and compared using Gray's test accounting for competing risks.
Results: Across the years (1984-2018), the median age was 50.0 (range: 18-76) with 59.6% of the patients being male. Acute myeloid leukemia accounted for 36.3% of transplants, followed by non-Hodgkin lymphoma (14.2%), acute lymphoid leukemia (11.8%), chronic myeloid leukemia (10.1%), and myelodysplastic syndrome (10.0%). Fifty-five percent of patients received myeloablative conditioning. Across the groups, statistically significant improvements in PFS and OS were observed (p<0.001 and p<0.001, respectively) (Figure 1a, 1b). The median PFS improved from 0.8 yrs. (95% confidence interval [CI]: 0.6-1.2) in gp 1 to 3.7 yrs. (95% CI: 2.3-NR) in gp 7. The median OS also improved from 1.0 yrs. (95% CI: 0.7-1.2) in gp1 to NR (95% CI: 4.2-NR) in gp7. The 5-yr PFS among the groups were 24, 25, 25, 28, 33, 41 and 48%, respectively, with a significant improvement seen since 2004. Similar improved trends were seen at 10 yrs. The 5-yr OS were 25, 28, 28, 28, 40, 47 and 53%, respectively, with similar significant improvement seen since 2004. Similar improved trends were seen at 10 yrs. Complete GVHD data was available since 1999 (gp 4-7). The cumulative incidence of grade II-IV aGVHD increased over the years: 36, 27, 38, and 52% at day 100 and 37, 31, 44, and 55%, respectively, at day 180 (Figure 1c). Grade III-IV aGVHD were 21, 10, 11, and 19% at day 100 and 22, 11, 13, and 21% by day 180, respectively, with the highest rate seen for groups 4 and 7. Overall cGVHD also increased over the 4 group years with day 365 cGVHD at 38, 40, 34, and 48% and extensive cGVHD at 27, 34, 31, and 44%, respectively (p<0.001 and p<0.001, respectively). The rate of NRM significantly improved across the years, with 1-yr NRM at 40, 38, 42, 46, 21, 15, and 15% and 5-yr NRM at 54, 51, 51, 57, 31, 22, and 24%, respectively, with a significant improvement seen since 2004 (Figure 1d).
Conclusion: Our data shows improved overall and progression-free survival post allo-SCT over decades, which may be attributed to advances in supportive care, and GVHD and relapse mitigation therapy. The decline in NRM is also likely due to improved supportive measures such as infectious disease monitoring and prophylaxis. Nonetheless, post-transplant relapse and grade III-IV aGVHD remain prominent challenges. Therefore, future research should continue to investigate therapeutic strategies that can both reduce high grade GVHD while limiting post-transplant relapse.
Chaudhry:Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees. Bumma:Amgen: Speakers Bureau; Sanofi: Speakers Bureau. Khan:Amgen: Consultancy; Janssen: Consultancy. Devarakonda:Janssen: Consultancy. Vasu:Kiadis Inc: Other: Kiadis has obtained exclusive licensing requirements from The OHio State University; Janssen: Membership on an entity's Board of Directors or advisory committees; Omeros: Membership on an entity's Board of Directors or advisory committees. Jaglowski:CRISPR: Consultancy; Novartis: Consultancy, Research Funding; Juno: Consultancy; Kite, a Gilead Company: Consultancy, Research Funding. William:Incyte: Research Funding; Guidepoint Global: Consultancy; Dova: Research Funding; Merck: Research Funding; Seattle Genetics: Research Funding; Kyowa Kirin: Consultancy, Honoraria; Celgene: Consultancy, Honoraria. Mims:Leukemia and Lymphoma Society: Other: Senior Medical Director for Beat AML Study; Agios: Consultancy; Abbvie: Membership on an entity's Board of Directors or advisory committees; Syndax Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Other: Data Safety Monitoring Board; Kura Oncology: Membership on an entity's Board of Directors or advisory committees; Novartis: Speakers Bureau. Brammer:Bristol-Myers Squibb: Research Funding; Celgene: Research Funding; Seattle Genetics: Honoraria, Speakers Bureau; Kymera: Honoraria; Verastem Oncology: Other: Travel. Saad:Incyte Pharmaceuticals: Other: Personal Fees; Amgen: Other: research support; Kadmon: Other: research support; Orcabio: Other: research support; Magenta Therapeutics: Other: Personal Fees. Efebera:Celgene: Research Funding; Takeda: Honoraria, Speakers Bureau; Pharmacyclics: Research Funding; Ohio State University: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.